Introduction
The claims process is a pivotal moment in the intricate web of insurance operations. It’s the juncture where policyholders seek reimbursement for covered losses and damages, and insurers assess and settle these claims. Traditionally, this process has been laden with paperwork, manual data entry, and prolonged wait times. However, the advent of claims process automation is revolutionizing this fundamental aspect of the insurance industry. In this blog, we will explore claims process automation, examples of claims processes you can automate, the benefits of using claims process automation, and a lot more.
What is Claims Process Automation?
Claims Process Automation is the implementation of technology and software solutions to streamline and optimize the handling of insurance claims. It involves the automation of various tasks and steps involved in the claims processing workflow, such as data entry, document verification, decision-making, and communication with policyholders, healthcare providers, or other stakeholders.
Automating Claims Processing aims to improve efficiency, accuracy, and speed in processing insurance claims while reducing manual intervention and the potential for errors. It typically involves the use of intelligent algorithms, machine learning, optical character recognition (OCR), and workflow automation tools to handle claims more efficiently.
Overall, Claims Process Automation is a vital component of modern insurance operations, helping insurance companies process claims faster, enhance customer satisfaction, and reduce operational costs.
Challenges in Manual Claims Processing
Government regulations and penalties, coupled with a constantly growing volume of claims, exacerbate the status quo that many insurers face – like slower resolution times that frustrate customers and soaring operational costs caused by error-prone data handling. Let’s look at the challenges faced by insurers in brief-
-
Heavy Operational Cost
Keeping costs in check is always at the top of the list while modernizing traditional claims processing. When systems all across the organization are not integrated, the claims agent must have to look across multiple systems and sources to find the right information rather than apply his decision-making to settle the claims. Also, insurer agents also have to re-key the information between system or emails, CRM, and backend applications. This approach introduces errors, frustration, and additional costs.
A recent study found that only 5% of insurers are fully digitized or automated. -
Lack of Consistent Delivery
It is common for manual claims processing to lack consistency and efficiency in task management. A customer may be dissatisfied when an insurance agent calculates different payouts for identical claims. Furthermore, if one claim is given priority over another without proper time management, delays and inaccuracies can occur.
-
Poor Data Integration
In claims processing, data integration is the technical process of combining data derived from multiple sources and creating a centralized system. Additionally, the main concern with data is dealing with inaccurate and outdated data. A single error in the system leads to customer dissatisfaction and errors in initiating the claims payment that further leads to a dissatisfied customer experience.
According to a recent survey, only 30% of policyholders reported a positive experience with their insurance providers. -
Increasing Claims Fraud
As per the report, insurance claims fraud estimates loss is $308.6 billion in the year 2022. Such malicious claims add up to extra strain on insurance agents as a lot of time must be dedicated to analyzing the authenticity of claims. And if analyzed manually it takes a long time to check the authenticity and chances of errors as well. This is another reason that almost 78% of consumers are concerned about insurance fraud.
-
Rising Customer Expectations
When it comes to customers, convenience, and communication are at the top of the list. Also with rising online claims management insurers’ agents are expected to be available 24/7 to answer customer queries. And with more innovative players entering the market policy pricing and quality is not the only enough to retain customers.
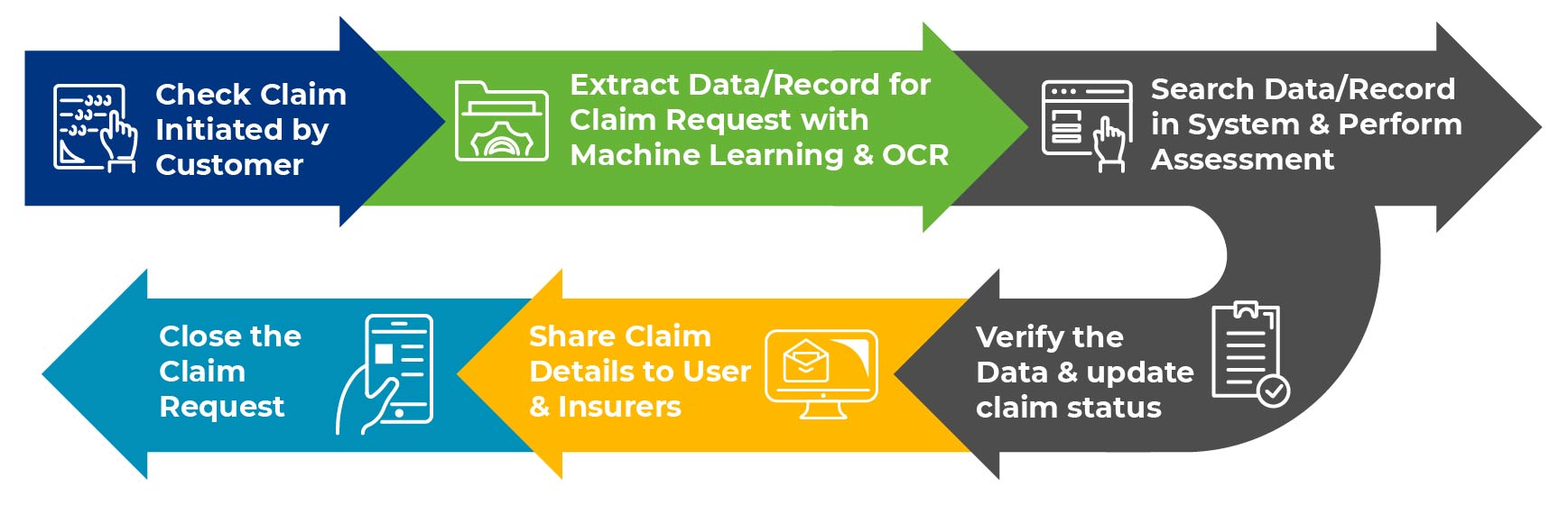
How Claims Process Automation Works?
Claims processing involves a series of steps before claims payment is transferred to the customers. Using automation technologies like RPA in insurance claims processing a lot of tasks are involved in the claims process. Let’s see how automated claims processing work.
-
Data Entry
To initiate the claims process, insurers’ agents had to go through a lot of paper trails, emails and pdfs to extract data to check the claims information. Reporting and processing this whole data into a claims management system, requires a lot of focus and attention. In this process, using intelligent RPA bots can automate the data entry task and reduce the chances of errors and speed up the claims processing.
-
Claims Verification
As soon as the data is entered into the claims management system, insurers’ agents have to go through a thorough assessment of claims documents initiated by users. Insurers also have to make sure that every data that is collected are accurate, matches the regulatory compliance, and is not duplicated. RPA in insurance claims processing can cross-verify and check the claims data against relevant database and rules and determines the amount of compensation that is payable. Going automation way, insurance agents can potentially detect fraud and reduce the time required to process claims
-
Claims Adjudication
After claims verification, RPA can help insurance agents in determining the eligibility of claims by comparing them against the pre-determined rules set by insurers. Claims process automation can easily flag claims that require attention and ensure that claims are adjudicated accurately and efficiently. Also, an RPA chatbot can help in appealing for claims in case claims are denied.
-
Claims Settlement and Communication
As soon as claims data is verified and settlement is done, insurance agents need to communicate with policyholders for sending out notifications and reminders. Here instead of humans sharing information, RPA bots can be leveraged to share information. This rules out the requirement of offering operational availability 24/7 for claims processing and reduces the workload for humans.
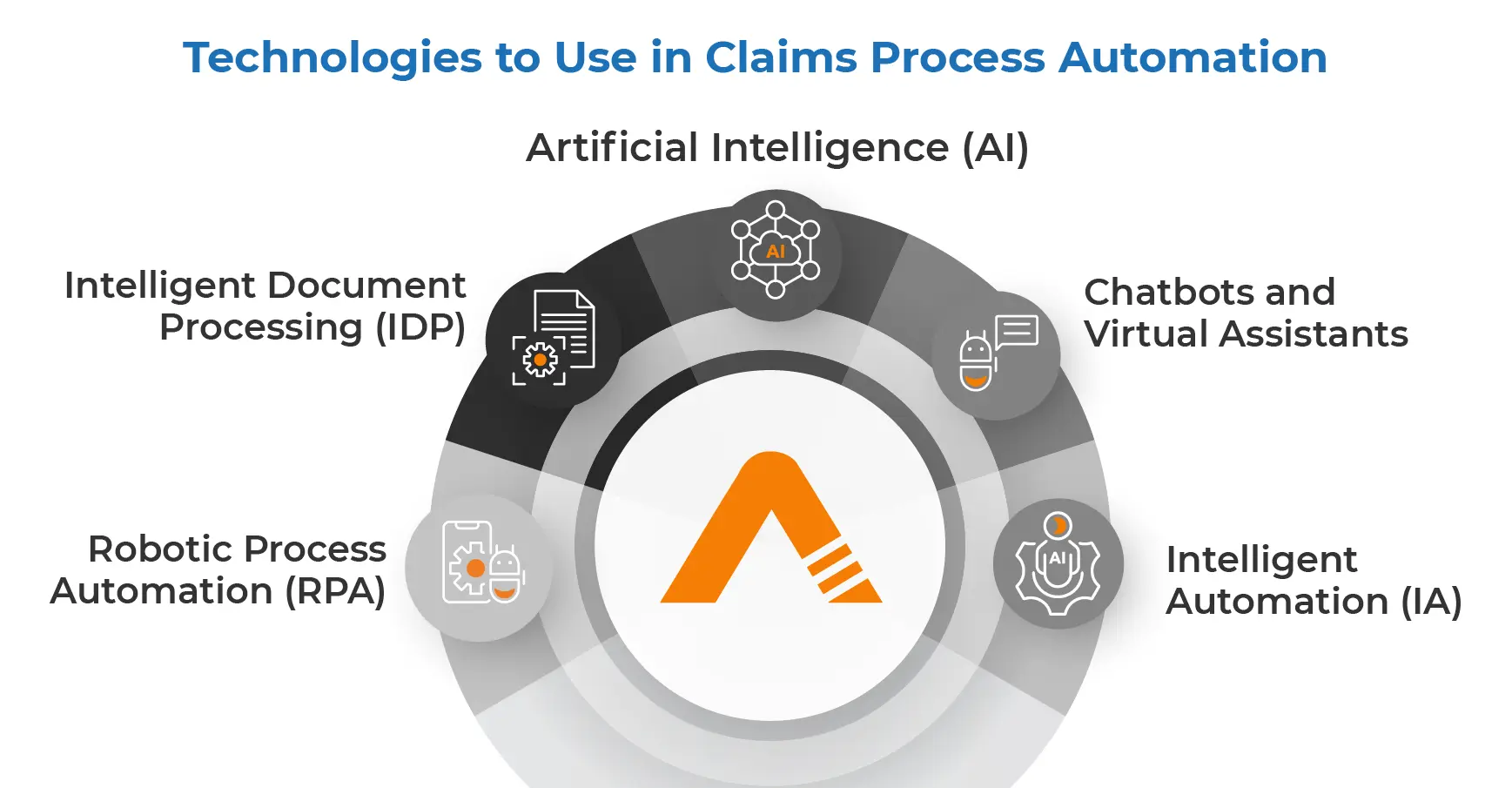
Technologies to Use in Claims Process Automation
Insurers looking to automate claims processing can leverage a combination of technologies tailored to their specific needs and operational requirements. Each technology brings unique capabilities and benefits to streamline different aspects of the claims lifecycle. Here’s a breakdown of key technologies and their roles in claims processing automation:
-
Intelligent Document Processing (IDP):
IDP solutions use advanced optical character recognition (OCR), natural language processing (NLP), and machine learning algorithms to extract relevant information from unstructured documents such as claim forms, invoices, and supporting documents. IDP helps insurers automate data capture, validation, and classification, reducing manual data entry and accelerating claims processing workflows.
-
Robotic Process Automation (RPA):
RPA software robots emulate human actions to automate repetitive, rule-based tasks within the claims process, such as data entry, document verification, and status updates across multiple systems and applications. RPA enhances operational efficiency, reduces errors, and streamlines end-to-end claims handling, enabling insurers to improve productivity and scalability.
-
Artificial Intelligence (AI):
AI-powered algorithms enable insurers to leverage predictive analytics, pattern recognition, and anomaly detection to optimize claims decision-making, detect fraudulent activities, and forecast claim outcomes with greater accuracy. AI algorithms can analyze vast datasets, identify emerging trends, and provide actionable insights to claims adjusters, enhancing operational agility and risk management capabilities.
-
Intelligent Automation (IA)
Intelligent Automation integrates AI, RPA, and cognitive technologies to orchestrate complex workflows, automate decision-making, and optimize resource allocation within claims operations. IA solutions enable insurers to design end-to-end automation processes, dynamically adapt to changing business conditions, and deliver personalized customer experiences across digital touchpoints.
-
Chatbots and Virtual Assistants:
Chatbots and virtual assistants powered by AI and natural language understanding (NLU) technologies enable policyholders to initiate claims, track claim status, and obtain assistance through conversational interfaces across digital channels such as websites, mobile apps, and messaging platforms. Chatbots enhance customer engagement, reduce call center volumes, and provide round-the-clock support, enhancing the overall claims experience.
By integrating these technologies into their claims processing workflows, insurers can achieve significant improvements in efficiency, accuracy, and customer satisfaction. However, successful implementation requires careful planning, stakeholder collaboration, and ongoing optimization to maximize the value of automation investments and drive sustainable business outcomes in the evolving landscape of insurance.
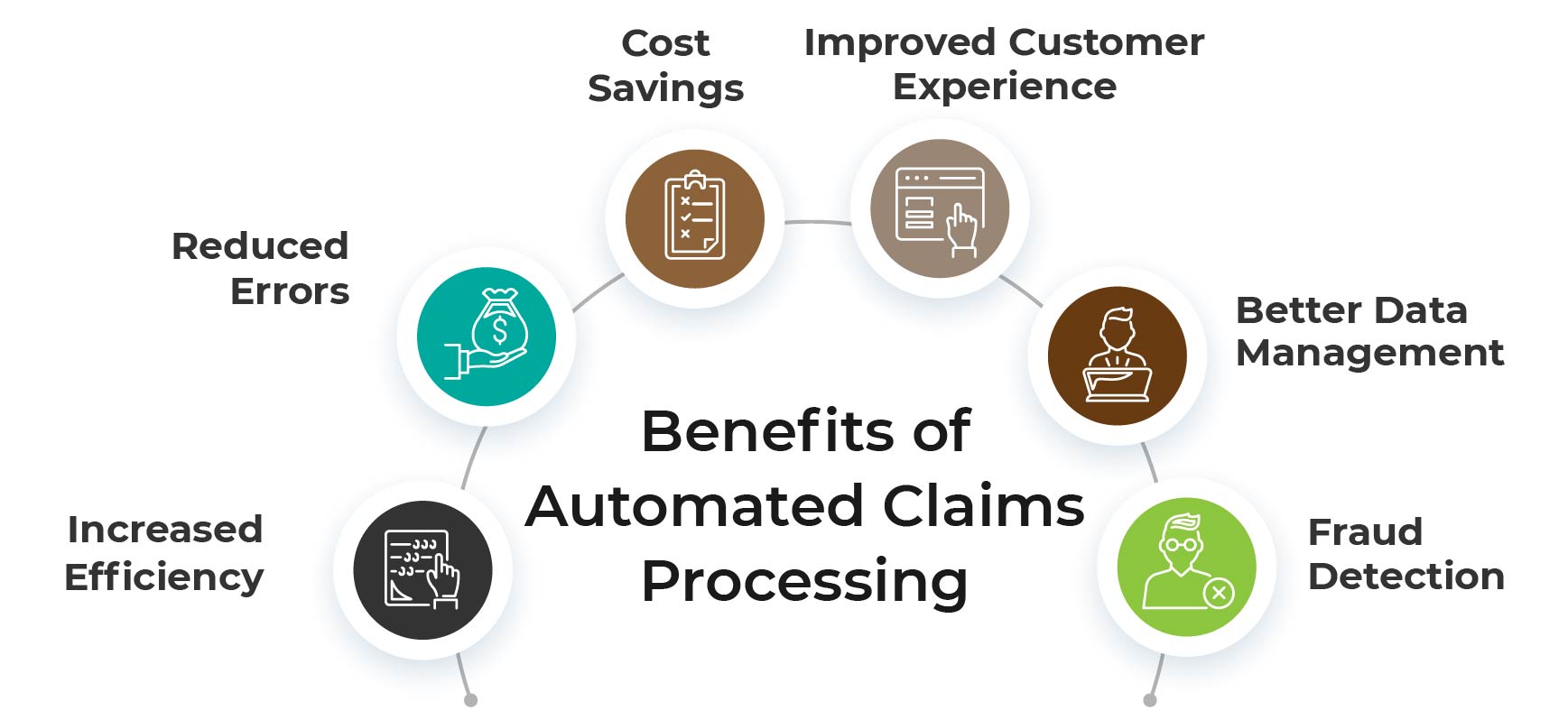
Benefits of Automated Claims Processing
Automated claims processing can bring several benefits to insurance companies, including
-
Increased Efficiency
Claims processing automation can reduce the time and effort required to process claims. This means that claims processing is done more quickly, and resources can be allocated more efficiently.
-
Reduced Errors
Using intelligent RPA bots can minimize the risk of errors and omissions. This can help to ensure that claims are processed accurately and that claimants receive the appropriate compensation.
-
Cost Savings
Having RPA bots take care of the data reporting and verification tasks can reduce the cost of claims processing. As cost is reduced, insurance agents can better use the money for implementing RPA solutions in other insurance processes.
-
Improved Customer Experience
Automated claims processing can improve the customer experience by reducing processing times and providing faster and more accurate claims decisions. This can help to increase customer satisfaction scores and make sure these customers stay longer with your organization.
-
Better Data Management
Integrating intelligent document processing into claims processing can significantly enhance data management. These bots are adept at capturing and storing data in a structured and organized manner, making it easier to analyze information and identify valuable patterns that can be utilized to optimize claims processing.
-
Fraud Detection
Automated claims processing can also help to detect fraudulent claims by using machine learning and artificial intelligence to identify anomalies and inconsistencies in claims data.
[Also Read – RPA in Insurance: Benefits, Use Cases & Challenges 2024]
Conclusion
As customer needs change rapidly and competition increases, insurers continue to face challenges. Furthermore, insurers have begun implementing RPA in back-office processes to automate transactional, routine, rule-based tasks during which capital and talent are repurposed to address more complex and strategic challenges. Using robotic process automation in insurance can promote long-term success and productive market opportunities. Due to its versatility and advantages, automation will undoubtedly be adopted in the insurance sector as well.
