Given the increasing challenges hospice providers face, such as staffing shortages and resource constraints, how can we ensure that patients continue receiving high-quality end-of-life care? AI in hospice care is emerging as a transformative force across industries. However, adoption rates vary significantly between sectors. While many industries are rapidly integrating AI, with an estimated 86% of companies implementing the technology, the home health and hospice sector lags. Studies indicate that less than 3% of organizations in this field have embraced AI solutions, suggesting a considerable gap in technological adoption.
This display highlights both an opportunity and a challenge for home health & hospice agencies. So, how can home health & hospice agencies benefit from using AI and improve patient care? Let’s find the answer in this blog and explore how Artificial Intelligence can be used in hospice care.
AI in Hospice Care- A Potential Solution to Reshape Hospice Care
The hospice and post-acute care industry faces ongoing regulatory challenges, resource limitations, and staffing concerns. Despite this, caregivers remain passionate and committed to providing quality, timely care. In hospice, where every moment is crucial, clinicians support patients and families through an emotionally and spiritually intense journey. Given these challenges, innovation is essential, pushing beyond traditional medical practices. Holistic strategies are needed to enhance care, ensuring comfort, peace of mind, and a better patient and caregiver experience.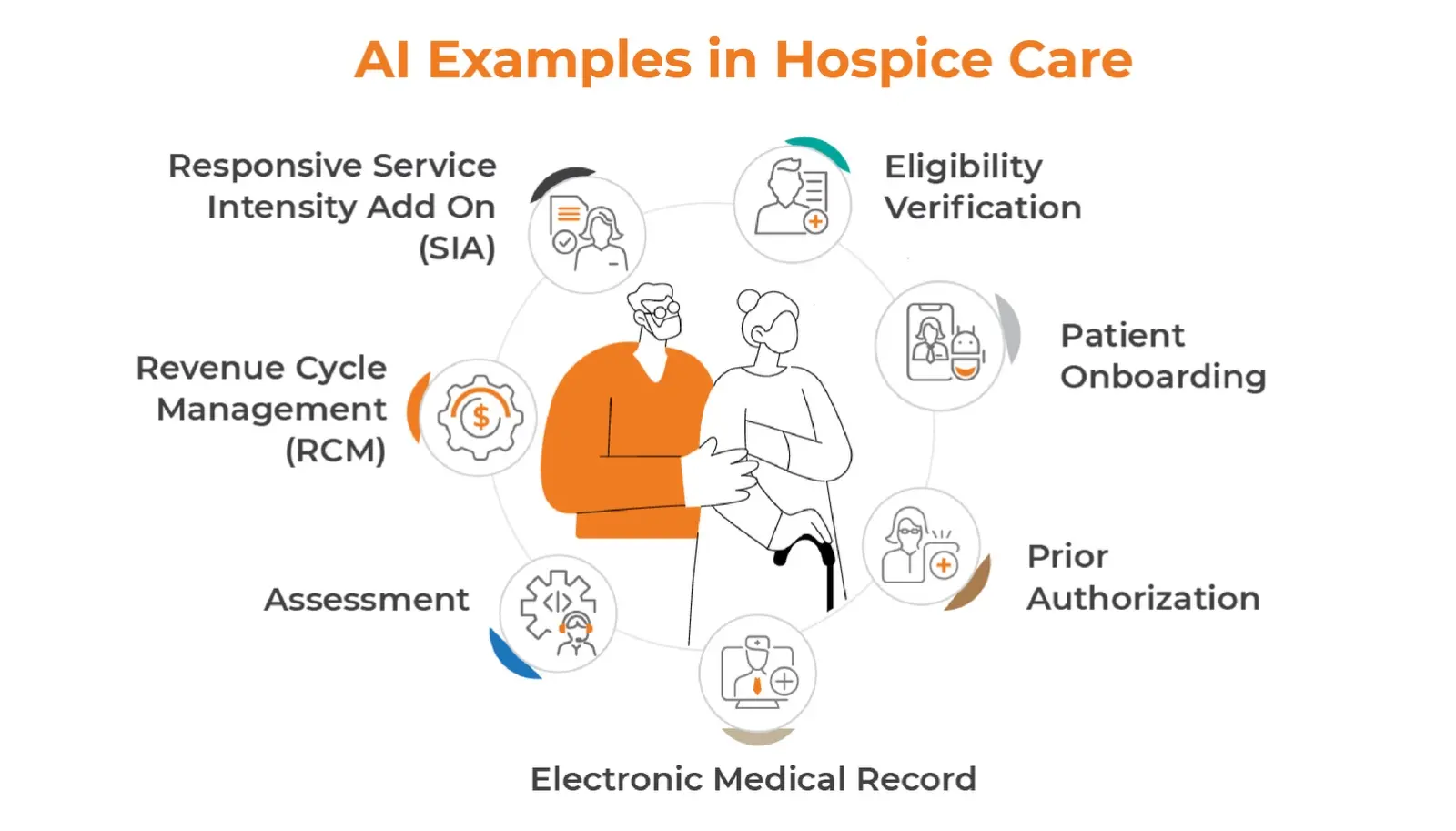
AI in hospice and palliative care solutions providers can be of great help. Per a hospice news survey, a hospice organization achieved 97% increased patient visits due to implementing AI in hospice. That’s huge. Implementing AI in hospice care can address challenges faced by hospice, such as clinician shortages, resource limitations, and other administrative tasks. Let’s explore some compelling potential hospice use cases that not only save time and money but also enhance overall operational effectiveness-
-
Eligibility Verification
Eligibility verification is a multi-step process that typically requires multiple logins to different systems to verify a single patient’s information. When done manually, this process can consume many hours each week, delaying patient care.
AI in hospice care solutions simplifies this process through intelligent document processing, addressing the challenges of insurance verification and helping healthcare providers initiate timely care while ensuring accurate reimbursements. With hospice care solutions, organizations can-- Extract patient insurance details, such as member ID and date of birth, from scanned cards using OCR and machine learning.
- Automatically verify insurance eligibility through insurance portals.
- Update the information in EHR systems and share the verification status.
-
Patient Onboarding
Patients in hospice care are typically referred for in-hospital by their attending physician, requiring services to begin immediately. However, onboarding in-hospital patients involves complex coordination across multiple functions such as time tracking, charting, billing, coding, and claims processing. The manual process is slow and prone to data-entry errors due to the high data integration and processing volume.
With a simplified data-entry interface, the intake team and referring physician collaborate to input the patient’s medical data, including diagnoses, demographics, insurance details, and relevant circumstances. AI in hospice care can then:
- Identifies follow-up admission tasks and required face-to-face visits.
- Assign the appropriate care team based on location.
- Prepares the patient’s electronic medical record.
- Generates draft clinical notes for the care team to review and submit.
This approach fastens the patient onboarding process and enhances the coordination between teams.
-
Prior Authorization
On average, 78% of physicians stated that delay in prior authorization leads to treatment abandonment. The manual approach leads to delayed care and patient dissatisfaction, which ultimately forces home & hospice agencies to look for AI in hospice process. Automate prior authorization in hospice, extract essential patient information and analyze payer policies to determine if requests meet approval criteria, ensuring alignment with best practices.
Additionally, automated systems enable the electronic submission of prior authorization requests, facilitating real-time processing and immediate decision-making. This automated system in prior authorization eliminates long waiting periods and generates approvals or denials based on predefined rules. That’s how AI in hospice care expedites treatment plans by minimizing manual reviews and enhancing the overall patient care experience.
-
Electronic Medical Record
Hospice care faces unique challenges in automating electronic medical records (EMRs) due to the complexity of patient needs, varied care settings, and the highly personalized nature of care. Integrating diverse data points like clinical notes, medication management, and emotional or spiritual care requires sophisticated systems that align with hospice workflows.
Data interoperability is a crucial feature of the EMR system. EMR automation enables the creation of comprehensive and centralized patient records in hospice care, encompassing medical histories, treatment plans, medication records, and advance care directives. These records are not only easily accessible but also simplify the information-gathering process.
Streamlining documentation reduces the risk of errors while allowing healthcare professionals to access vital information quickly. This is particularly important in hospice care, where timely decision-making and accurate data are critical for delivering the highest quality of care.
-
Assessment
Leveraging deep-learning-powered AI for assessments transforms the accuracy and efficiency of care planning. Clinicians experience faster assessments and more precise diagnoses as AI generates personalized care plans, completes OASIS questions, and identifies additional diagnoses. This reduces coding costs and minimizes the need for in-person reviews, significantly boosting operational efficiency. The streamlined process enhances the quality of care and improves clinician satisfaction, allowing them to focus more on patient needs while reducing administrative burdens.
-
Revenue Cycle Management (RCM)
RCM automation in hospice care can significantly reduce errors and streamline the revenue cycle by automating key processes such as patient intake, insurance verification, and claim submission. One critical area is verifying Medicare Part A coverage and identifying any secondary insurance, such as Medicaid or private insurance, to ensure claims are sent to the correct payer in the proper order. Automating these tasks helps avoid billing errors and denials due to incorrect assumptions about coverage.
By reducing manual data entry, RCM automation minimizes common mistakes, such as misspelling patient names, entering incorrect birth or death dates, and using outdated payer or Medicare Beneficiary Identifier (MBI) numbers. Accurate automation of certification and recertification dates ensures that benefit periods are adequately covered. Ultimately, RCM automation strengthens hospice revenue cycle management, reducing denials and improving cash flow by eliminating simple intake errors and expediting the billing process.
-
Responsive Service Intensity Add On (SIA)
The Service Intensity Add-on (SIA) is a crucial aspect of hospice care, providing additional financial support for patients with complex needs. This add-on recognizes the increased resources and effort required to care for these individuals effectively. But, the challenges that come with SIA management are-
- Difficulty in tracking care intensity
- Ensuring qualified staff for intensive care
- Coordinating effectively between teams
- Balancing staff workload and patient needs
By utilizing advanced algorithms, AI can analyze medical codes inputted by RNs to determine a patient’s status, categorizing it as either “normal” or “SIA” (Serious Incident Alert).
When a patient’s status is flagged as SIA, the automated system promptly alerts the patient’s direct care team, ensuring they receive immediate notifications. This rapid response capability facilitates timely interventions and significantly enhances the overall quality of patient care. Ultimately, AI in hospice care contributes to better health outcomes and can increase revenues by optimizing operational efficiency and resource allocation.
Way Forward
Integrating AI in hospice care will also bring new ethical considerations to the forefront. Industry leaders will need to grapple with questions about:
- The appropriate balance between human touch and AI-driven care
- Ensuring AI decisions align with patient values and preferences
- Maintaining the human element in end-of-life care
As we embrace the future of hospice care solutions, it’s clear that AI and automation will play a crucial role in shaping a more efficient, compassionate, and patient-centered approach to end-of-life care. By thoughtfully integrating these technologies, we can create a future where hospice care is not only more effective but also more accessible and personalized to each individual’s needs.
