Most home healthcare agencies don’t lose clients because of poor care — they lose them before care even begins. A critical factor is home health EMR intake, often dismissed as routine data entry—is the backbone of every home healthcare operation.
At the heart of it all lie home healthcare EMR intake forms — deceptively simple, yet deeply impactful. Each field plays a role: mandatory fields ensure compliance and accuracy, while optional fields reveal insights that personalize care and enhance client experience.
With AI-powered patient intake automation, agencies can streamline, validate, and auto-populate these forms — transforming intake from a bottleneck into a strategic advantage.
In this blog, we’ll explore the balance between mandatory and optional intake fields, why it matters more than you think, and how AI can intelligently streamline, AI’s role in optimizing accuracy, and best practices that boost compliance, care quality, and client satisfaction.
“In-home healthcare, getting the intake right means getting care right from the very first step”
What are Mandatory vs Optional Fields in Home HealthCare?
In-home healthcare, the intake process is where each client relationship begins, and that’s the only place where things can go wrong or right. A well-designed home healthcare EMR intake doesn’t just capture the information it builds the foundation of compliance, coordination, and quality care.
But not all the intake fields serve the same purpose. It’s essential to understand the difference between mandatory and optional fields, as this helps agencies streamline operations without sacrificing personalization —a balance crucial for home healthcare onboarding.
Mandatory Fields: The Non-Negotiables
Mandatory fields in home healthcare intake are the backbone of compliance and clinical readiness. home healthcare agencies must capture these details to meet the regulatory standards and start the service without delay.
Typical examples of mandatory fields include:
| Field Type | Description | Purpose |
|---|---|---|
| Demographics | Full name, date of birth, address, and contact details. | Critical for accurate identification and clear communication |
| Emergency Contacts | Contact information for family or designated emergency individuals. | Ensures staff can reach the right person quickly in an urgent or crisis situation |
| Consent Forms | Authorizations for treatment, data usage and release of information | Ensures legal compliance and protects both the agency and client through proper consent |
| Insurance Details | Policy information, coverage verification, and billing-related data | Ensure accurate billing and reimbursement and prevent payment delays |
| Medical History | Diagnoses allergies, medication and primary physician information | Offer the foundation for safe, informed and personalized care delivery |
When these fields are incomplete or inaccurate, everything downstream — from billing to care planning — becomes vulnerable. For agency owners, this means potential compliance risks, payment delays, or even service interruptions.
Optional Fields: The Personal Touch
Optional fields are not required by regulation, but they are often what make you stand out. They help your team understand your client beyond their chart, as a person with preferences, habits and needs that shape their daily experience.
| Field Type | Description | Purpose |
|---|---|---|
| Language Preferences | The client’s preferred language(s) for communication. | Promotes comfort, understanding, and stronger relationships between clients and caregivers. |
| Dietary Needs | Specific meal preferences, restrictions, or allergies. | Ensures caregivers plan meals that align with health requirements and cultural norms. |
| Cultural Considerations | Information about traditions, customs, or faith-related care practices. | Builds trust through respect and personalized, culturally sensitive care. |
| Transportation Needs | Details about mobility challenges or transport requirements for appointments and errands | Helps coordinate logistics efficiently and support client independence. |
| Hobbies or Interests | Activities or interests that bring the client joy and comfort. | Enhances emotional well-being and helps caregivers create meaningful engagement |
These optional fields might seem “extra,” but for many agencies, they’re the secret to higher client satisfaction and caregiver engagement. They turn service into connection — and that’s where long-term loyalty begins.
A: Optional fields, like language preferences or dietary needs, help personalize care and boost client satisfaction.
What are the Stakeholder Challenges with Home Healthcare Intake?
The Home Healthcare EMR Intake process may look simple — collect information, enter it into the system, and start care. But for most agencies, this is where complexity begins. Every stakeholder — from agency owners to caregivers — faces unique challenges that can affect efficiency, compliance, and client satisfaction.
Here’s how those challenges play out across the home healthcare ecosystem.
-
For Agency Owners
Home health intake is more than just form billing; it’s a foundation for compliance, finance, and operations. When data in the Home Health Intake Form Template is incomplete or inconsistent, the ripple effects are immediate and costly.
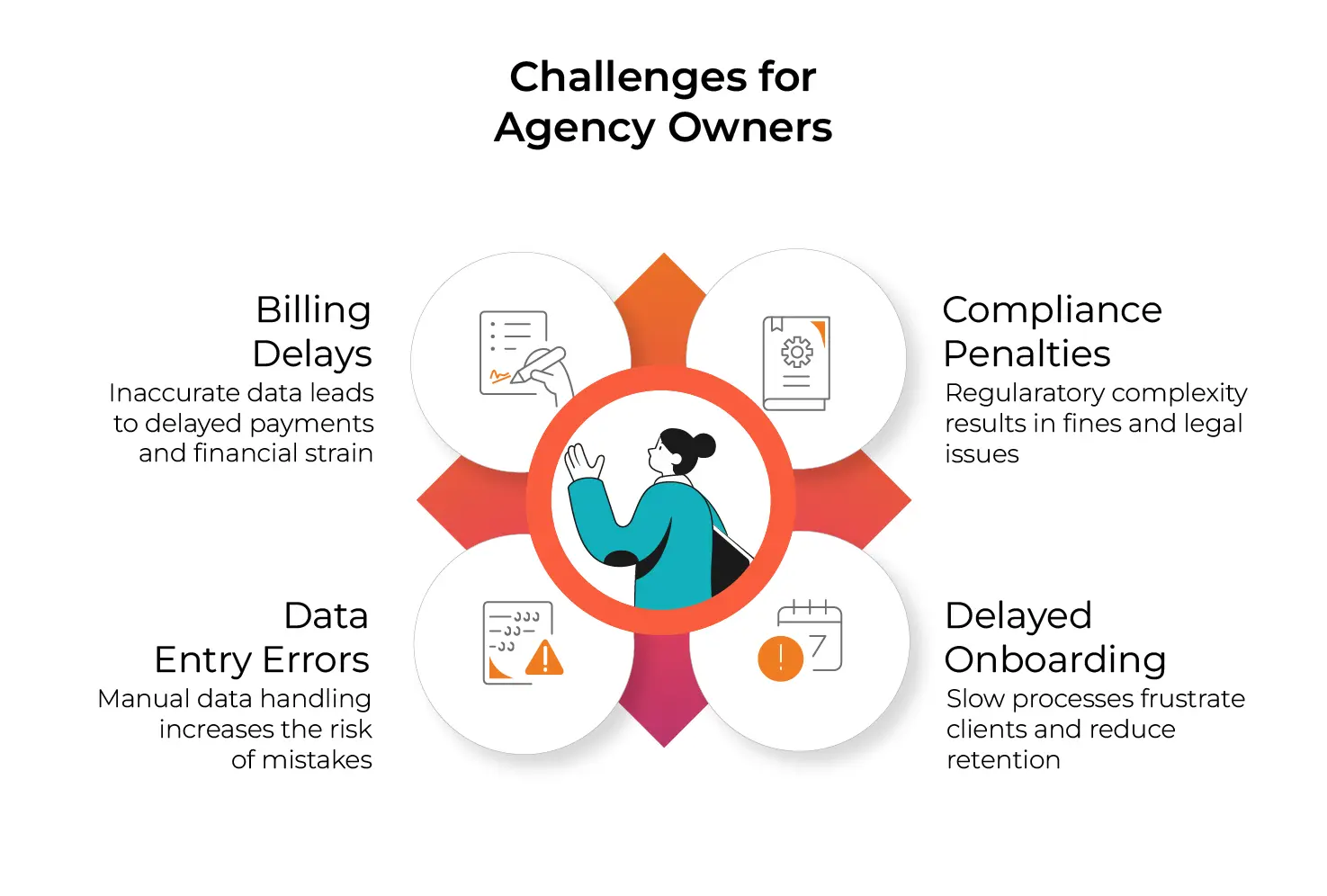
According to the Home Care Technology Report (2024), 27% of claim denials in home care stem from incomplete or inaccurate intake documentation.
-
For Staff & Administrators
Administrative staff are at the center of the Patient Intake Automation challenge — responsible for juggling paperwork, calls, and digital documentation under tight timelines.
Staff spend up to 40% of their day on documentation and manual data handling (Source: NAHC)
-
For Caregivers: Information Gaps & Unclear Care Plans
Caregivers rely on accurate, timely Home Health Intake information to deliver safe and consistent care. When the home healthcare EMR Intake process is incomplete, caregivers often face gaps in understanding a client’s needs.

A Home Health Care News survey found that 38% of caregivers received incomplete client information before their first visit — leading to care inconsistencies
-
For Clients & Families
For clients and families, Client Onboarding is their first experience with your agency — and it sets the tone for everything that follows. A confusing or repetitive process can erode trust and delay care.

-
Regulatory Changes, Workflow Confusion, and Patient Impact
- Studies highlight that frequent regulatory updates and bureaucratic license processes create confusion, resistance, and delays for home healthcare agency owners and staff. These barriers also slow the registration of new agencies, increasing competition stress and limiting patient access to new providers.
- For patients, repeated intake questioning and incomplete documentation can delay the start of care and contribute to frustration. The administrative burden of accessing care often leads to delayed service initiation and lower satisfaction ratings.
How AI Helps Streamline EMR Intake?
The EMR intake process has traditionally been one of the most time-consuming, error-prone parts of home healthcare operations. From filling out referral details to uploading client documents, every step demands precision — and every missed field or mismatch can delay care, affect compliance, or lead to billing denials.
That’s where AI-powered Patient Intake Automation is transforming the game. By embedding intelligence directly into intake workflows, home healthcare agencies can ensure that every form is complete, every record is accurate, and every team member is guided in real time.
Here’s a quick overview of how AI improves home healthcare EMR intake — at a glance
- Auto-validates mandatory fields in real time to prevent errors and ensure compliance.
- Extracts data automatically from referral forms, physician notes, and scanned documents using NLP and OCR.
- Provides intelligent guidance to staff during intake, flagging inconsistencies and missing information.
- Customizes workflows for each care plan type, ensuring relevant questions are asked.
- Integrates seamlessly with EMR, billing, and scheduling systems to eliminate duplicate entry.
- Enhances patient experience by reducing repetitive questions and speeding up onboarding.
While the bullet points above provide a quick snapshot of AI’s impact on home healthcare EMR intake, each of these benefits warrants closer examination.
Let’s explore how AI-powered solutions work step by step to validate data, automate extraction, guide staff, customize workflows, and integrate seamlessly — helping agencies save time, reduce errors, and deliver a better patient experience.
-
Smart Field Validation & Real-Time Reminders
An AI-powered solution for home healthcare can automatically verify that all mandatory fields — such as demographics, consent forms, and insurance details — are correctly completed before submission.
For example, if a staff member forgets to include a policy number or upload a signed consent, the system instantly flags the omission and prompts them with a reminder.
How this helps:- Prevents incomplete Home Health Intake Form Templates from reaching compliance risk.
- Reduces billing rejections caused by missing or inaccurate data.
- Ensures real-time accountability — no form can move forward unless critical details are captured.
Example: An agency using AI-driven intake validation saw an 80% improvement in process efficiency, which further helped in increasing their conversion rate by 20%.
Catch their Full Success Story Here -
Automated Data Extraction
Manual data entry has long been the bottleneck in Home Health Intake. AI eliminates this pain by using natural language processing (NLP) and optical character recognition (OCR) to automatically extract data from referral forms, physician notes, or uploaded documents.
Care coordinators can even dictate information via speech-to-text, and AI will transcribe and populate the right EMR fields.How this helps:
- Speeds up home healthcare Onboarding by reducing manual typing.
- Converts unstructured documents (e.g., scanned faxes, PDFs) into clean, structured EMR data.
Example: A major hospice network using AI-driven data extraction cut intake processing time from 45 minutes to under 10 minutes per client.
-
Real-Time Error Flagging & Intelligent Guidance
AI acts like a digital co-pilot during the Patient Intake Automation process — continuously checking for inconsistencies and providing real-time guidance to staff or clients completing forms.
If the client’s date of birth doesn’t match the insurance record, or a medication allergy field is left blank, the system automatically flags it before submission.
If the client’s date of birth doesn’t match the insurance record, or a medication allergy field is left blank, the system automatically flags it before submission.How this helps:
- Prevents costly intake errors and compliance risks.
- Guides intake coordinators through each step for accuracy.
- Reduces back-and-forth communication between staff and clients to fix missing data.
-
Customized Intake Workflows for Different Care Plans
No two clients are the same — and neither should their intake forms be. AI enables agencies to tailor EMR intake workflows according to the specific type of service (e.g., skilled nursing, hospice, personal care).
Instead of using a one-size-fits-all form, the AI dynamically adjusts required fields and checklists depending on the care plan.How this helps:
- Reduces staff cognitive load — they only see relevant questions.
- Ensures regulatory compliance for each care category (e.g., Medicare vs. private pay).
- Streamlines Home Health Intake by minimizing unnecessary data entry.
-
Seamless Integration Across Systems
AI-enabled home healthcare EMR Intake solutions integrate with existing EMRs, billing systems, and scheduling platforms, ensuring a single, unified source of truth.
Instead of staff manually entering the same information multiple times, AI synchronizes it across systems in real time — from intake to billing to care coordination.How this helps:
- Eliminates duplicate data entry.
- Ensures consistency across all records and reports.
- Improves visibility for caregivers and administrators alike.
What’s Next: AI Trends in Home Healthcare Patient Intake?
AI is already transforming home healthcare intake, but the next wave promises even smarter, faster, and more personalized workflows. Emerging technologies and advanced algorithms are set to enhance accuracy, compliance, and patient satisfaction like never before.
Here’s what agencies can expect in the near future.
- Predictive Analytics for Patient Risk Identification
AI will analyze intake data to predict potential care risks, flagging patients who may need extra attention even before the first visit. - Voice-Assisted and Speech-to-Text Intake
Intake forms can be completed verbally, with AI transcribing and auto-populating EMR fields in real time — reducing manual typing errors and time. - Hyper-Personalization of Intake Forms
AI will dynamically suggest optional fields based on client profiles, including dietary preferences, cultural considerations, and mobility needs, enhancing patient-centered care. - IoT Integration for Real-Time Data Capture
Intake workflows will connect with wearable devices or remote monitoring tools, automatically updating EMRs with patient vitals, medication adherence, and activity data. - Semantic AI for Smarter Data Classification
AI will interpret unstructured data from documents, notes, or emails and automatically categorize it into relevant EMR fields, improving accuracy and decision-making.
A: AI complements staff, automates repetitive tasks, and enhances accuracy, but human oversight remains essential for care decisions.
Best Practices and Tips for Home Healthcare Agencies
| Focus Area | Key Insight | Practical Application / Tip | Impact on Operations |
|---|---|---|---|
| Determine Which Intake Fields Should Be Mandatory vs. Optional | Not all client information carries the same compliance or care importance. | Classify fields in your Home Health Intake Form Template into mandatory (compliance-critical) and optional (personalization-focused). | Reduces compliance risk and data overload while improving care personalization. |
| Mandatory Fields | Essential for compliance, safety, and billing accuracy. | Include demographics, insurance details, medical history, emergency contacts, and consent forms. | Ensures regulatory adherence, accurate billing, and timely service activation. |
| Optional Fields | Builds stronger client relationships and personalization. | Capture language preferences, dietary needs, and cultural considerations when relevant. | Enhances satisfaction, retention, and caregiver-client trust. |
| Incorporate Digital & AI Tools | Manual data entry is inefficient and error-prone in modern home healthcare. | Adopt AI-powered digital intake to automate data capture, validation, and task management. | Increases accuracy, saves staff time, and supports compliance. |
| Enable Real-Time Status Tracking | Lack of intake visibility causes delays and missed follow-ups. | Utilize AI dashboards to monitor intakes that are pending, incomplete, or approved. | Improves home healthcare Onboarding speed and workflow transparency. |
| Personalize Workflows | One-size-fits-all forms slow down staff and confuse clients. | With Patient Intake Automation, dynamically adjust forms based on care type (e.g., hospice, skilled nursing). | Streamlines data collection and enhances relevance. |
| Integrate Systems | Fragmented platforms lead to duplication and data errors. | Connect your digital intake solution with your Home Health Intake EMR, billing, and scheduling tools. | Creates a single source of truth for faster, more accurate operations. |
Conclusion
In today’s fast-changing home healthcare market, the line between agencies that thrive and those that merely survive isn’t about size — it’s about efficiency and intelligence.
Your intake process is more than an administrative step. It’s the moment where compliance, compassion, and coordination either align — or fall apart.
A well-designed, AI-powered home healthcare EMR Intake system transforms this moment from a bottleneck into a breakthrough. It doesn’t just capture data — it creates clarity, speed, and confidence across your entire operation.
When agencies move from manual paperwork to AI-driven digital intake, they don’t just save time — they redefine what’s possible:
- Slash administrative burden so staff can focus on people, not paperwork.
- Eliminate errors and compliance risks before they ever reach billing or audits.
- Empower caregivers with accurate, real-time client information from day one.
- Accelerate home healthcare Onboarding while delivering a more personal client experience.
The message is clear — smart intake design isn’t just a back-office upgrade; it’s a competitive advantage. Because in-home healthcare, efficiency isn’t about doing more — it’s about freeing your team to care better.
Start with AI. Build a stronger, faster, more human agency from intake onward.