In the ever-evolving landscape of healthcare, technology continues to reshape various aspects of patient care and administrative processes. As per the report, the global robotic process automation in healthcare market is expected to hit around USD 14.18 billion by 2032 with a registered CAGR of 26.1% from 2023 to 2032. In our earlier blog, we discussed the Electronic health record management and how automation can simplify it.
In this blog, we will explore how insurance eligibility verification and benefits checks are important processes in the healthcare revenue cycle once a patient schedules an appointment. So let’s explore more about patient insurance eligibility verification and how automation can fast-track the verification process for healthcare providers.
What is the Patient Insurance Eligibility Verification Process?
Patient insurance eligibility verification plays a pivotal role within the realm of medical billing, as it is an essential step to ensure the seamless progression of procedures.
It involves the process of confirming whether a patient possesses valid and active insurance coverage at the point when they require medical attention. Moreover, this process extends to verifying the intricate details of their insurance policy.
In addition, it is important to understand what treatments are covered by the policy, what limitations exist, and what exceptions or prerequisites must be met before the insurance company assumes responsibility for a particular medical service. This process involves four steps that must be performed by healthcare providers to complete the process and these steps are-
Results of Incorrect or Delayed Verification of Insurance Eligibility
Failure to perform precise and prompt insurance eligibility verification can lead to various challenges for healthcare providers.
-
Delayed Reimbursements
healthcare providers do not verify a patient’s insurance coverage promptly and accurately, there’s a risk that the services provided may not be covered by the patient’s insurance policy. This could result in the provider submitting a claim to the insurance company, only to have it rejected. As a result, the reimbursement for the services rendered would be postponed. Providers might need to pursue payment directly from the patient or absorb the costs themselves.
-
Claim Rejections
In cases where insurance coverage isn’t adequately verified, healthcare providers might offer services that are not covered by the patient’s insurance plan. Consequently, when the provider submits a claim to the insurance company for these services, the claim could be turned down entirely. This leaves the provider without compensation for the services they’ve delivered.
-
Operational Inefficiencies
Addressing each denied claim necessitates extra administrative work, whether it entails pursuing payment from the patient or absorbing the cost. This added administrative burden contributes to operational inefficiencies and increased operational costs.
AutomationEdge to Streamline Patient Insurance Eligibility Verification Process
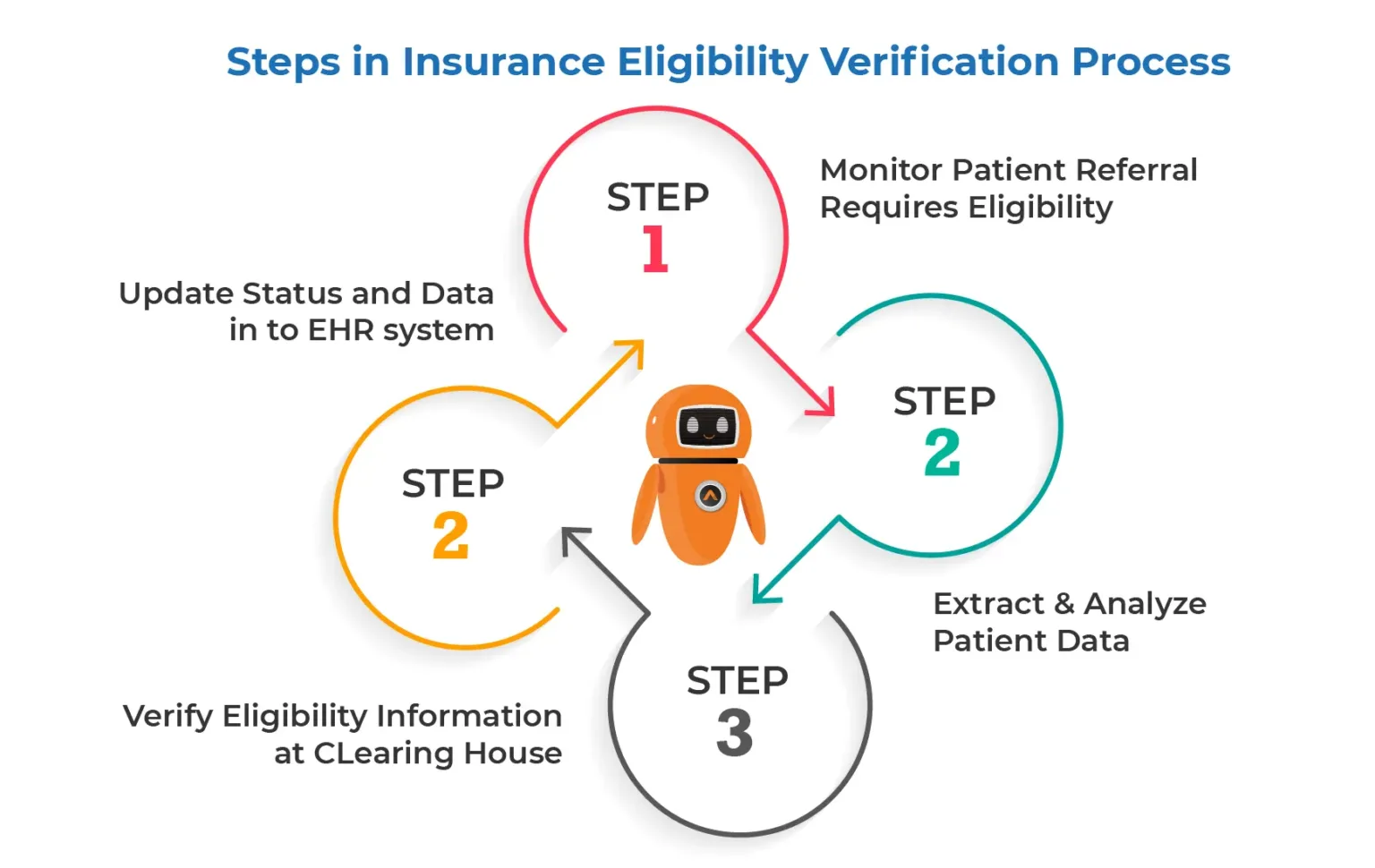
Insurance eligibility verification is a multi-step process that requires multiple logins to disparate systems of record to verify information given by a single patient. When done manually, this process could consume numerous hours within a week, significantly impeding prompt patient care.
AutomationEdge’s AI solution comes with intelligent document processing capabilities that can address the insurance eligibility verification challenges and help healthcare providers. It eliminates the necessity of navigating various record systems to initiate timely care and ensure accurate reimbursements. Using AutomationEdge’s AI bot enterprises can-
- Read the patient insurance information using OCR, and Machine Learning(ML) like member ID and Date of Birth from the scanned card
- Check the insurance eligibility on the insurance portal using automation
- Update the information in EHR systems and share the status
Automated insurance eligibility verification processes reduce queue time and improve customer experience. This also enables front desk staff to have more time at hand to work on patient queries. Most importantly, it ensures the accuracy of patient and insurer information while onboarding new patient referrals.
Conclusion
Automating the process of verifying patient insurance eligibility holds a multitude of advantages for healthcare providers. These encompass heightened precision, streamlined efficiency, reduced expenses, and elevated patient contentment.
Despite potential obstacles, the integration of automated verification stands as a judicious approach for healthcare providers striving to update their practices and amplify their fiscal viability. As technological progress persists, we can envisage additional refinements in automated verification systems, thereby amplifying their efficiency, precision, and security.
Frequently Asked Questions (FAQs)
It extracts and updates coverage details directly into your system. This reduces manual work, speeds up intake, and minimizes claim denials.
Insurance eligibility verification automation systems instantly check a patient’s coverage by connecting with insurance databases in real-time.
They verify plan details, co-pays, and deductibles without manual input. This reduces errors, saves time, and speeds up the intake process.
Insurance verification is automated using technologies like AI, RPA (Robotic Process Automation), and OCR (Optical Character Recognition).
These tools extract, validate, and update insurance details in real time. This reduces manual work, minimizes errors, and speeds up patient onboarding.
Other Articles in the Series
- What is RPA in Healthcare?
- Why Should Healthcare Providers Choose Automated Patient Scheduling?
- Why Use Automation in Admission and Discharge Process in Healthcare?
- How Does Automated Patient Referral Process Work?
- Automating Testing Requests and Report Management in Healthcare
- Transform Patient and CareGiver Experience with Electronic Visit Verification Automation (EVV)
- Improving Electronic Health Record Management with Automation
- Simplifying Healthcare Insurance Claims Processing with RPA
- What is Medicare Payment Process Automation in Healthcare?
- Accelerating Revenue Cycle Management with AI-Powered Automation