More than half of the medicare beneficiaries are now in MA plans- and now they are demanding proof, not just promises.
What if payers suddenly demanded proof of outcomes—not just visits—before sending patients your way? In 2025, with Medicare Advantage enrolling 55.4% of beneficiaries and CMS expanding Home Health Value-Based Purchasing (HHVBP) nationwide alongside a proposed 6.4% payment cut, that future is here.
Home health agencies that rely on fee-for-service are at risk of being cut out of preferred networks. On the other hand, value-based agencies are gaining traction and creating growth opportunities. This shift leads to better patient outcomes and adds more comfort and calm. And this approach requires new metrics, new thinking and new tools. In this blog, we will explore what value based care home health care means and how agencies must act on it to achieve it.
How Value-Based Care Works in Home Health Agencies
So, what is value- based care? In simple language, the value-based care home health model means “Agencies get rewarded for delivering better outcomes- not for doing more visits.”
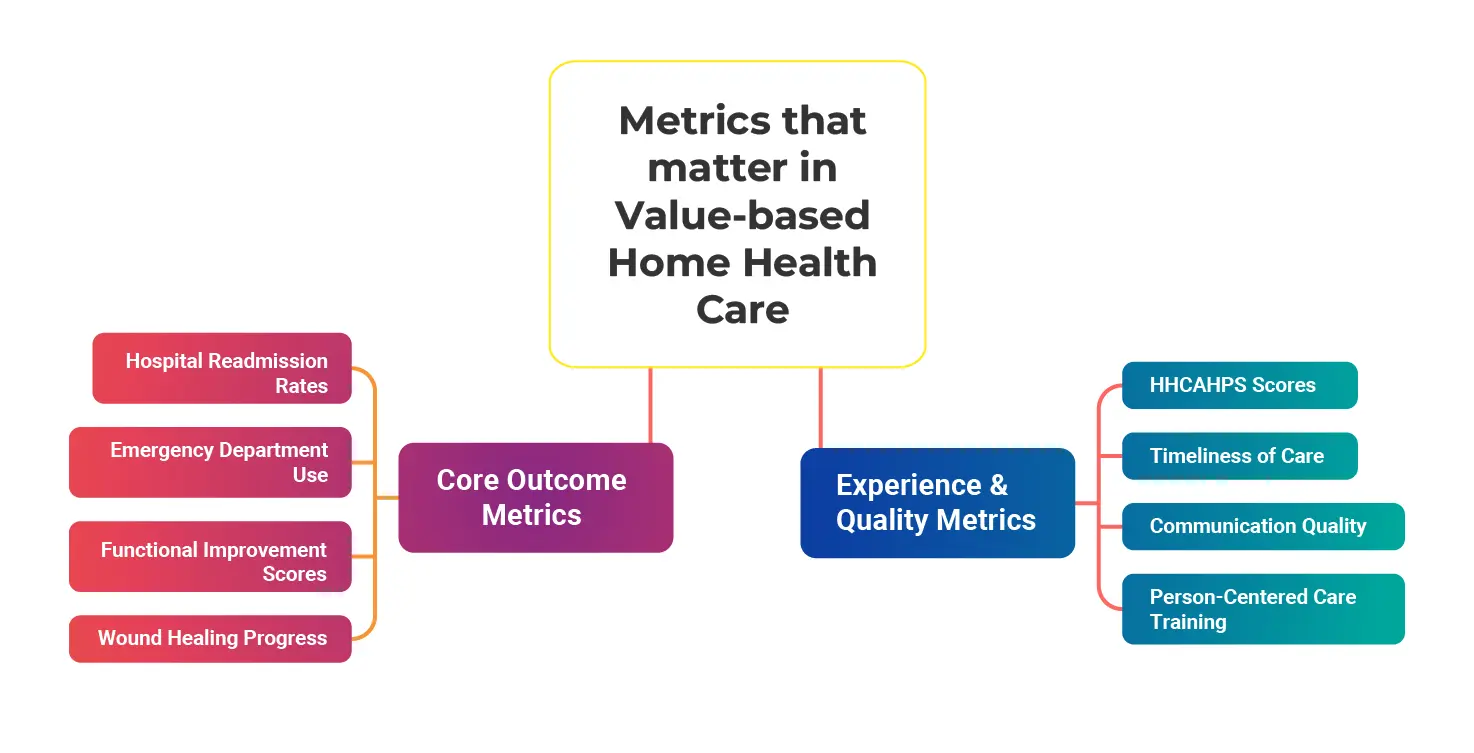
Instead of being paid based on volume, value-based models focus on:
- Patient outcomes (How well did the patient improve?)
- Total cost of care (Did the care plan prevent unnecessary hospital use?)
- Patient experience (Did the patient feel supported, safe, and satisfied?
When agencies help patients recover faster, avoid hospitalization, and have a better experience, they earn higher ratings—and stronger payer relationships.
Here is the list of bundled payment models for home health agencies :
| Model | What it Means | Why it Matters for Agencies |
|---|---|---|
| MA Value-Based Contracts | MA plan pays based on quality + cost performance, not visits. | More referrals and bonuses for high performers; lower or restricted referrals for low performers. |
| Shared Savings | Agencies share financial rewards if they help reduce total spending while improving outcomes. | Direct revenue upside for reducing hospitalization and enhancing care experience. |
| Episodic Bundles | One payment covers an entire episode of care (e.g., 30 or 60 days). | Force agencies to manage resources efficiently while also improving results. |
| Preferred Networks | Payers send referrals only to agencies meeting preset quality thresholds. | High-quality agencies gain more volume, while low performers lose market access. |
Why is the Value-Based Care Model Unavoidable?
For home health agencies, value based healthcare is not a trend anymore. The forces driving this transition are reshaping how payers choose partners, how agencies get reimbursed, and ultimately, which organizations grow versus which ones fall behind.
-
Macro Driver
Across the country, payers are moving rapidly toward models that reward outcomes over volume. Two major shifts are accelerating the change:
- The rise of managed Medicare and Medicaid
Medicare Advantage enrollment has surged, and managed Medicaid is expanding across states. These plans care deeply about one thing: keeping members healthier while reducing avoidable utilization. To achieve this, they’re seeking home health partners who can:- Prevent unnecessary hospitalizations
- Reduce emergency department visits
- Improve overall patient function
- Fee-for-service(FFS) Pressure
Traditional FFS home health continues to face reimbursement pressure, making it harder to grow without demonstrating higher measurable value.
This pushes agencies to differentiate through:- Stronger patient experience
- Higher quality data reporting
- More-efficient cre delivery
- The rise of managed Medicare and Medicaid
-
Competitive Dynamics Are Shifting Rapidly
Payers, ACOs, and health systems are no longer looking for “any” home health provider. They are building networks based on performance, not geography.
Here’s what they care about most:- Readmission rates – Can your agency keep patients out of the hospital?
- Functional outcomes (OASIS) – Are patients actually improving under your care?
- Patient satisfaction and trust (HHCAHPS) – Do patients feel safe, informed, and supported?
- Care coordination – Do you communicate clearly with hospitals, physicians, and caregivers?
Core Challenges that Agencies Must Overcome
Before a home health agency adopts value-based care, it’s crucial to overcome the challenges. These core challenges include:
-
Workforce Shortage and Burnout
In a survey, around 59% of home care agencies in 2025 reported ongoing workforce shortages, with recruiting and retention named the top challenge by almost half of agency executives. This shortage is driven by soaring demand—U.S. home care workforce needs are expected to grow by over 34% between 2019 and 2029 to keep pace with aging populations.
Also, immigration policies and limited pipeline capacity worsen the caregiver shortage, forcing agencies to deploy their staff more efficiently and creatively.
-
Technology and Data Gaps
Many home health providers continue to rely on outdated technology systems, resulting in fragmented data. Increased security risks and a lack of real-time visibility lead to lower patient outcomes and operational performance.
Without home care documentation tools, accurate remote patient monitoring (RPM) agencies struggle to demonstrate the value-based metrics payers require for contract negotiation and reimbursement. This tech gap undermines the ability to coordinate care, intervene proactively, and optimize workflows.
-
Culture and Skills
Around 77.4% of providers reportedly train staff in person-centered care, yet only 51.9% of employees feel fully prepared to meet the complex and evolving needs of new clients. Many clinicians and frontline marketers still focus on “visits delivered” as a success metric rather than “outcomes achieved,” creating a cultural barrier to value-based performance.
Shifting mindset and skills from volume-centric to outcome-oriented requires targeted education and reinforcement. This can help in creating care aligned with the core goals of capability, comfort, and calm for patients.
How AI Solution Drives Value-Based Home Health Care
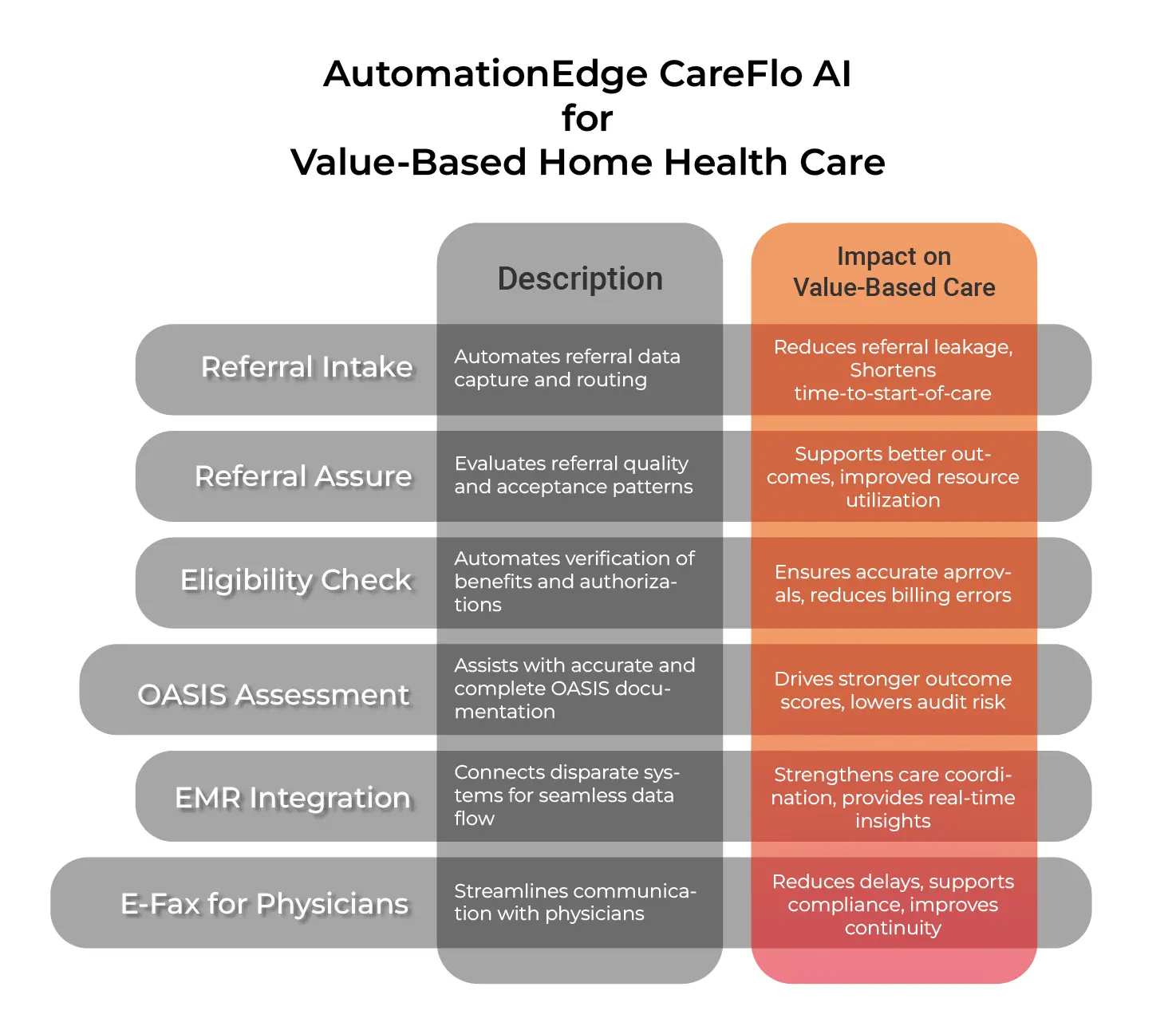
AI and automation in home health agencies can help create value based care by automating process that enhance patient care. Here are some areas where AI can help create a value-based care model for home health agencies.
-
Referral Intake & Triage
In a value-based care model, every referral matters; any delay or missed referrals can impact outcomes and revenue. Delays or missed referrals can directly harm patient outcomes and negatively impact revenue. AI can transform manual referral intake into an automated intake process that ensures the right patients are accepted at the right time.
Where AI fits:
- Intelligent Referral Intake
AI evaluates each referral instantly, factoring in clinical risk, payer type, geography, and staff availability to help agencies prioritize cases with the highest impact or urgency.For example, AutomationEdge has helped Bridge Home Health implement a 24/7 CareFlo AI assistance for referral intake. And this further increases its referral conversion rate by 20%. - Automated eligibility and authorization
AI powered eligibility and authorization works by instantly extracting patient and insurance details, logging into payer portals, and checking coverage in real time.The automated system submits required authorizations with the correct clinical documentation and tracks their status. As approvals are returned in minutes, it dramatically shortens time-to-start-of-care and removes the intake bottlenecks that slow agencies down. - Instant Referral Summaries
An AI-powered referral assure summarization solution can extract key details from long documents, PDFs, and faxes, identify the clinical information and organize it into structured data. As clinicians get a clear snapshot of history, diagnoses, meds, and risks in seconds, they can make faster, more confident acceptance decisions.
- Intelligent Referral Intake
-
Clinical Documentation
AI in home care documentation can improve the extraction and processing of clinical documents. Using intelligent tools like signature matching and eligibility checks helps agencies to improve the precision of their OASIS assessments and verification process. Technologies like NLP can further enhance documentation quality by identifying gaps and inconsistencies that affect compliance and reimbursement.
-
Care Coordination and Monitoring
An AI solution in home care supports proactive, value-based care by analyzing EMR data and predictive models to identify patients at elevated risk of deterioration. This enables earlier intervention and more coordinated care. Automated alerts and task routing also ensure timely responses to missed visits, abnormal vital signs, or concerning patient-reported outcomes. That further helps agencies reducing readmissions with a value-based home health care model.
-
Workforce Management and Engagement
AI solution improves workforce deployment and engagement by optimizing schedules and routes based on patient needs, caregiver skills, geographic constraints, and workload balance. This enhances productivity and ensures patients receive the right care from the best-suited clinician. Additionally, solutions like AI staffing help assign training and track completion, reinforcing person-centered competencies.
Final Thoughts
Value-based home health care is ultimately about giving people what they need most at home—comfort and patient care. It’s not just about cutting costs or chasing shared savings. It’s about helping patients feel safer, supported, and more independent.
When teams have the right tools and clear insight, they can focus more on meaningful interactions and less on paperwork. Home health agency adopting value-based care will be better positioned to grow, adapt, and make a lasting difference in the future of home health.
This is how value-based care becomes more than a payment model—it becomes a way of delivering care that honors patients’ dignity, strengthens caregiver relationships, and builds operational excellence.
