Are you a home health leader feeling the pressure of the Review Choice Demonstration (RCD)? Are you grappling with questions like:
- How can my agency stay compliant without drowning in paperwork?
- What does RCD mean for my patients’ access to timely care?
- Is this just another regulatory hurdle, or is there a silver lining?
You’re not alone. The RCD program, introduced by the Centers for Medicare & Medicaid Services (CMS), has sparked concern and curiosity across the home healthcare industry. Designed to reduce improper payments and ensure Medicare compliance, RCD automation is reshaping how home health agencies operate. But with change comes opportunity.
This blog explains review choice demonstration implications for home healthcare leaders like you, explores its challenges and benefits, and provides actionable strategies for surviving and thriving under this new framework. Let’s dive in!
Understanding Home Health Review Choice Demonstration Process
The Review Choice Demonstration is a CMS initiative to reduce fraud, waste, and abuse in home health services. It requires home health agencies in participating states (like Illinois, Ohio, and Texas) to demonstrate compliance with Medicare rules before or after receiving payment.
Think of it as a “quality check” for home health services. While the program’s intent is noble—ensuring patients receive necessary, high-quality care—it has added a layer of complexity for agencies already juggling tight margins and staffing challenges. As per the report, effective from June 1, 2024, CMS will be extending the Home Health Review Choice Demonstration Services for an additional 5 years.
The Key Objectives of RCD Automation include–
- Reduce improper payments by ensuring compliance with Medicare’s billing rules.
- Promote accountability in home health service delivery.
- Enhance patient protection through rigorous home care review process.
The program helps CMS verify that services are necessary and meet established guidelines, safeguarding the integrity of the healthcare system and the quality of care patients receive.
RCD in Action- How the Process Works?
The Review Choice Demonstration program offers home health agencies flexibility by allowing them to choose how their claims will be reviewed. The options include:
-
Pre-Claim Review for Home Health (PCR)
Agencies submit documentation before billing to confirm compliance with Medicare guidelines. This proactive approach allows agencies to address issues before the claim is processed, ensuring smooth reimbursement.
-
Post-Payment Review
Claims are reviewed after payment has been made. However, agencies that choose this option face a 25% payment reduction, which is only recoverable if they demonstrate a high compliance rate.
-
Opt-Out Option
Agencies can choose to forgo pre-claim and post-payment reviews but will be subject to a 100% review of all claims, increasing administrative complexity and risk.
Why is the Review Choice Demonstration Process Challenging for Home Health?
Here are some common pain points that home health agencies deal with are-
-
Varied Review Choices:
RCD automation offers providers multiple options, including pre-claim review, post-payment review, or a combination. However, this flexibility can complicate provider comparisons, as the review processes lack standardisation.
-
Complexity in Data Collection:
Tracking data accurately across different review modalities—such as review requests, claim denials, appeals, and provider responses—poses significant challenges. This complexity can lead to inconsistencies or inaccuracies in reporting.
-
Influence of External Factors:
Analysing the impact of home care review process becomes more complicated when external variables, such as shifts in patient demographics, changes in coding practices, or new regulatory updates, are considered. These variables can obscure clear conclusions.
-
Risk of Bias:
Providers may alter their practices in response to RCD, potentially skewing the data. Careful monitoring and analysis are required to ensure an unbiased interpretation of trends.
-
Delayed Data Accessibility:
Access to complete data sets may be delayed depending on the chosen review process. This lack of timely information can hinder practical analysis and decision-making.
AI & Automation Solution in Review Choice Demonstration Process
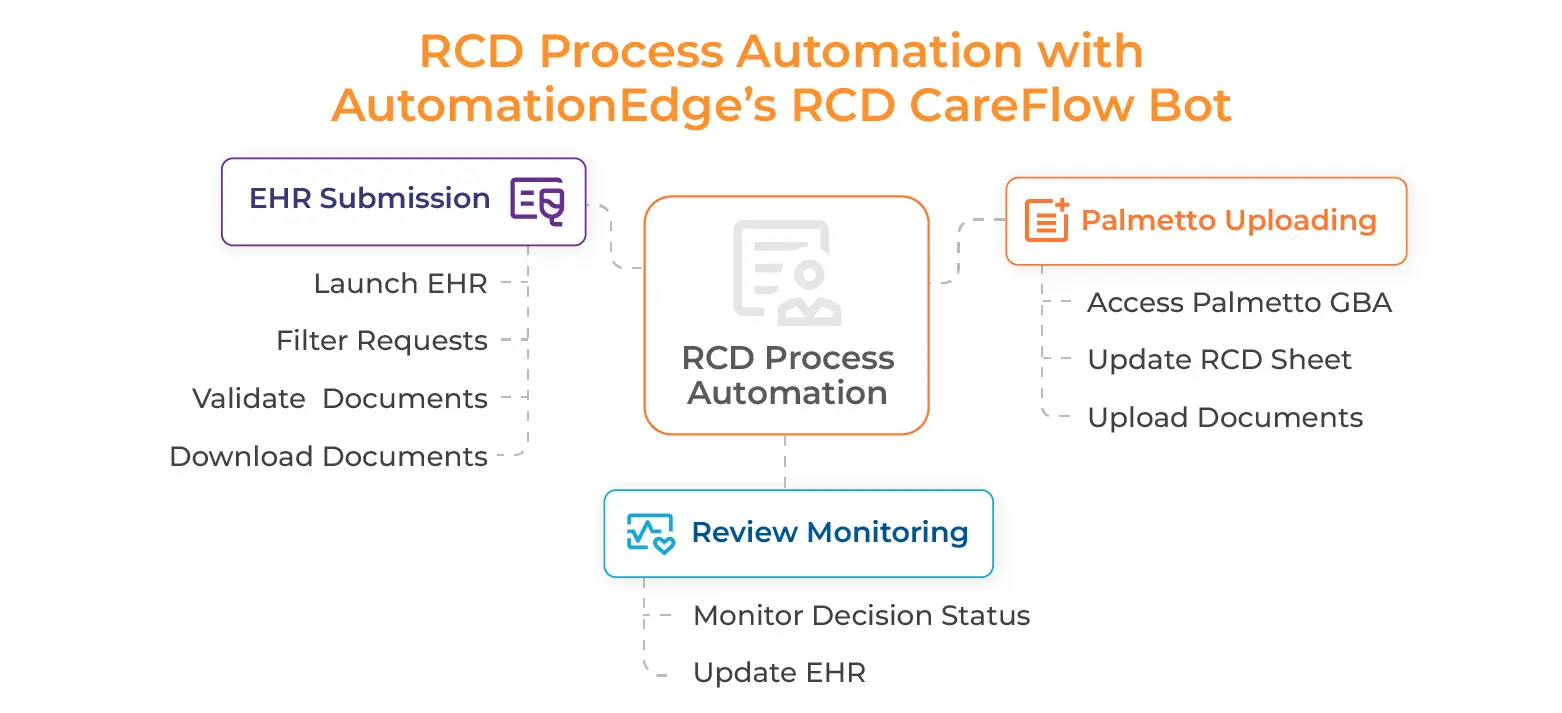
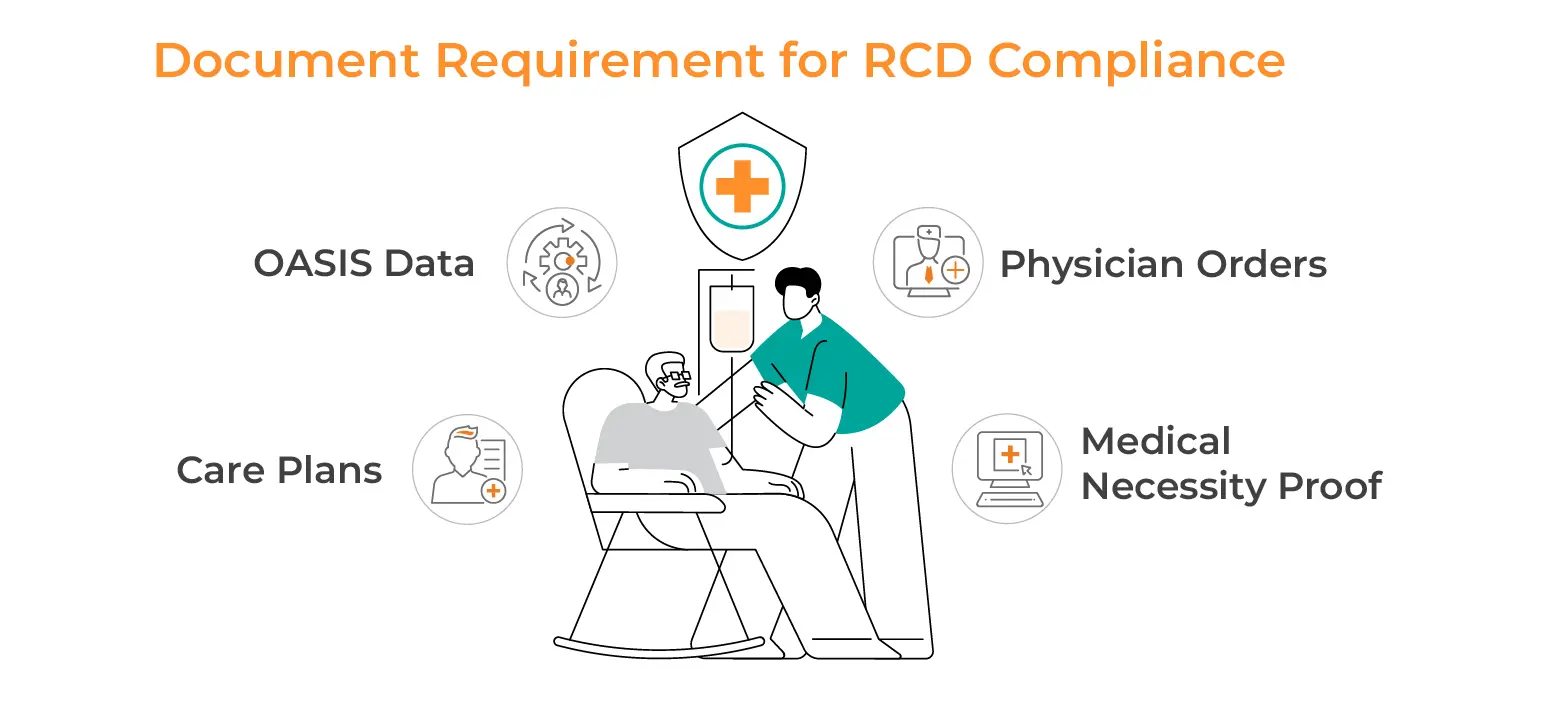
The Review Choice Demonstration (RCD) process is critical for home health agencies to ensure compliance with Medicare requirements while minimising claim denials and delays. However, it is also resource-intensive, involving multiple stages of documentation, validation, and status monitoring. By leveraging AI and automation solutions for home health RCD automation, agencies can streamline these steps, reduce errors, and save time and money. Here’s a detailed breakdown of how AI and automation can transform the RCD process and practical examples.
-
Streamlining RCD Submission in EHR
The first step in the home care review process is preparing documentation for submission, including completing the RCD sheet and ensuring all required forms are in order. AI-powered healthcare compliance solutions automate data entry, extracting patient details from the EHR systems, and populating the submission sheet. AI bots also perform real-time validation checks, ensuring key documents like CMS-485 forms are complete and alerting staff to missing or incomplete information for correction before submission.
-
Automating Document Uploads to Palmetto GBA
After preparing Pre-Claim review for home health submission sheet, the next task is uploading it and other required documents to the Palmetto GBA portal. This step is often time-consuming and prone to manual errors. However, automated home healthcare systems streamline this process by enabling seamless integration with the Palmetto GBA system.
Automation tools can log into the portal, navigate the necessary sections, and upload documents directly from the EHR. In addition, these tools ensure that the details in the Palmetto GBA portal align with the EHR records, preventing discrepancies.
-
Monitoring Review Status in Palmetto GBA
After submitting documents, agencies must track review outcomes, interpret results, and update the EHR. AI bot can streamline this by monitoring the Palmetto GBA portal in real-time and automatically processing outcomes like Provisionally Affirmative or Non-Affirmative. Bots retrieve decisions, update the EHR with the UTN and relevant details, and notify teams of the following steps: processing approved claims or flagging corrections for denied ones.
-
Reducing Operational Costs and Time
RCD automation significantly reduce the manual workload in home care review process, allowing agencies to process more claims quickly and accurately while ensuring compliance. Tasks like document verification and system updates that once took hours are completed in minutes, boosting efficiency and lowering costs. Automation minimises errors, avoids claim denials, and frees staff for higher-value activities like patient care.
-
Ensuring Compliance and Reducing Risk
Compliance with Medicare’s stringent guidelines is essential in the healthcare compliance solutions (RCD process), and AI ensures agencies meet these standards efficiently. AI-driven Pre-Claim review for home health systems validate submissions against Medicare’s rules, maintain detailed logs for audits, and scale to handle high claim volumes. By automating these processes, agencies reduce non-compliance risk and improve operational performance.
Conclusion
Navigating the Review Choice Demonstration (RCD) process can be complex, but it doesn’t have to be a barrier to efficiency or growth. By leveraging RCD automation and healthcare compliance solutions, home health agencies can transform compliance from a cumbersome regulatory burden into a streamlined, strategic advantage.
As CMS continues to evolve healthcare regulations, agencies that proactively integrate technology into their operations will stay ahead of compliance requirements while improving financial stability. The key to home health review choice process success isn’t just following the rules—it’s optimising them for efficiency and excellence.
Now is the time to embrace automation, stay compliant, and get paid faster. Is your agency ready to take the next step?
Frequently Asked Questions (FAQs)
If a home health agency fails to comply with RCD requirements, it may face penalties, including payment reductions or even loss of Medicare certification. Agencies must stay informed about the rules and adhere to them to avoid negative consequences.