Introduction
When Every Hour Matters, Documents Shouldn’t Delay Claims
Insurance claims often come at life’s most critical moments—a medical emergency, the sudden loss of a loved one, or an unexpected car accident. In these situations, policyholders are not just customers; they are people in distress, relying on their insurance provider for financial relief and emotional assurance.
But here’s the harsh reality:
- A family waiting for reimbursement of hospital bills spends days scanning, photocopying, and resubmitting documents because of missing details.
- A grieving spouse filing a life insurance claim struggles to provide a death certificate and FIR copy in the exact format required.
- A car accident victim is asked to submit odometer readings, RC books, and surveyor reports multiple times due to manual errors.
The result?
Claims get delayed by weeks, adding to emotional and financial stress.
According to an EY Insurance Survey (2024):
- 58% of claimants said document-related delays were their biggest frustration during claims.
- 72% of policyholders switch to competitors after a bad claims experience.
Most policyholders are not aware that insurers can now automate document processing for faster approvals. For insurers, automating document-heavy processes is no longer a choice—it’s an obligation to serve customers with empathy when they need it the most.
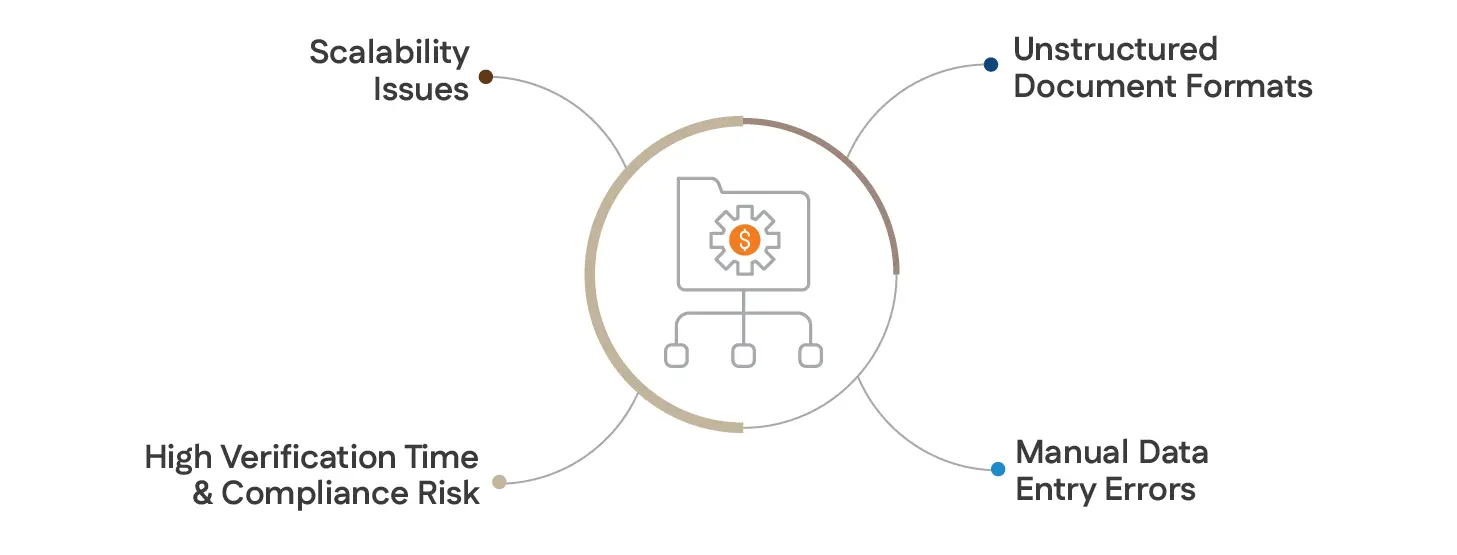
Big Challenge: Why Unstructured Documents Complicate Claims Processing Automation?
The insurance claims process is document-driven, and every claim type—health, life, or general—relies on a multitude of forms, medical reports, legal documents, and KYC proofs.
Here are the key pain points:
-
Unstructured Document Formats
- Customers submit documents in different formats: PDFs, scanned copies, handwritten forms, or even photos taken on mobile phones.
- Example: A health discharge summary may have a hospital logo, free-text diagnosis, and bill details embedded in tables—difficult for manual agents to interpret quickly.
-
Manual Data Entry Errors
- Insurance agents manually extract data like policy numbers, treatment costs, or KYC details, which leads to typos and mismatched records.
- A wrongly entered bank account number delays claim settlement or causes rejection.
-
High Verification Time & Compliance Risk
- Verifying FIR copies, postmortem reports, or RC books for motor claims can take days, as insurers need to cross-check them with government or hospital records.
- Any lapse risks fraudulent claims slipping through, costing millions annually.
-
Scalability Issues
- During peak seasons (e.g., natural calamities or pandemic waves), insurers are flooded with claims. Manual teams cannot scale fast enough to process thousands of documents.
Why Claim Document Automation Is Crucial for Faster Settlements
Document automation—powered by OCR (Optical Character Recognition), NLP (Natural Language Processing), and RPA (Robotic Process Automation)—transforms these manual tasks into seamless digital workflows.
Here’s why it’s no longer optional:

-
Faster Turnaround Time (TAT)
Automating document extraction and validation reduces claim processing time from weeks to hours. A health insurer can instantly extract diagnosis codes from discharge summaries and auto-approve low-risk claims.
-
Enhanced Accuracy & Fraud Detection
AI models can cross-check document data with government APIs or hospital systems, flagging fake death certificates or forged FIR copies.
-
Cost Savings & Scalability
Automation reduces manual intervention, cutting operational costs by 30–60% (Deloitte Insurance Report, 2024) and enabling insurers to process 10x more claims during surge periods.
-
Improved Customer Experience
A policyholder receiving claim approval within 24 hours builds trust and loyalty—critical in a competitive market.
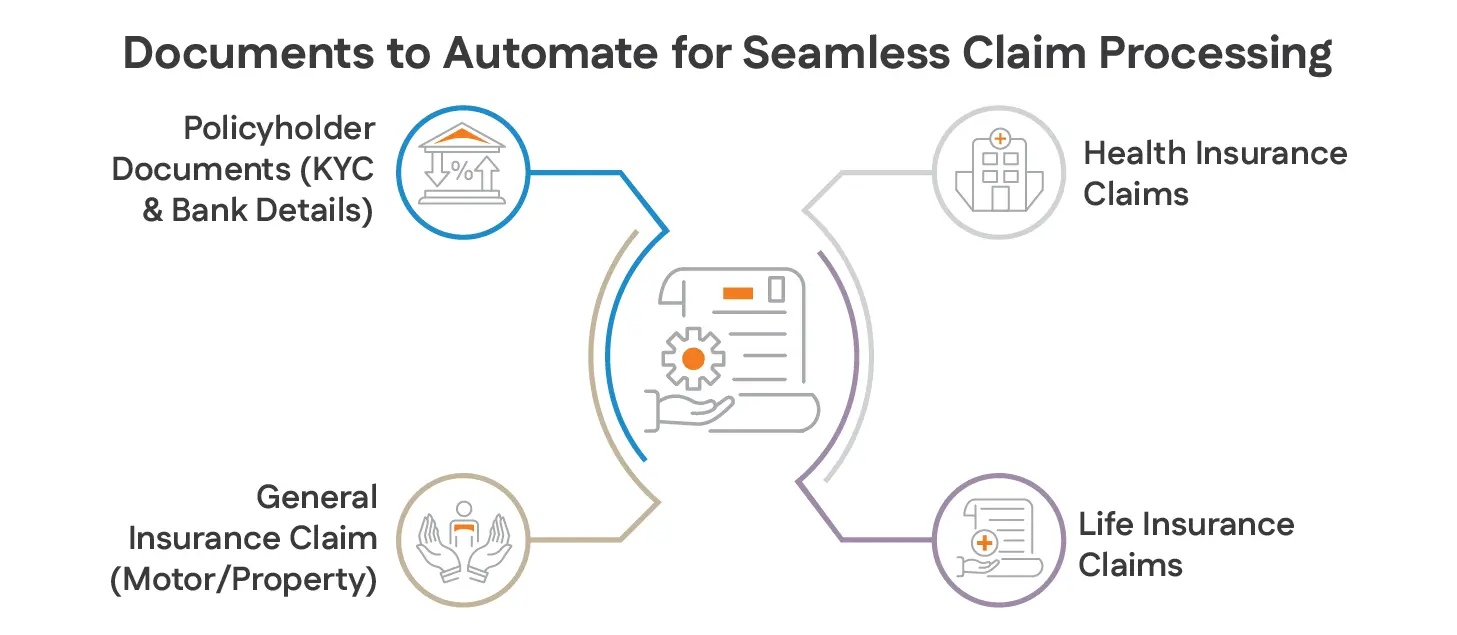
Documents to Automate for Seamless Claim Processing
The insurance claims process is document-driven, and every claim type—health, life, or general—relies on a multitude of forms, medical reports, legal documents, and KYC proofs.
-
Health Insurance Claims: Automating Claim Documents for Speed
Automating the following documents can help process claims faster and accurately:
- Claim Form
- Discharge Summary
- Inpatient Bills
- Investigation Reports
- Lab Reports
- Outpatient Bills (OPD Receipts)
AutomationEdge can extract diagnosis codes and treatment details from discharge summaries using OCR + NLP, match them against policy coverage, and auto-approve eligible claims.
-
Life Insurance Claims: Using Claim Document Automation to Reduce Errors
Life insurance claim processing can be tedious due to manual verification of multiple documents. Key documents to automate include-
- Claim Form
- Death Certificate
- FIR Copy
- Postmortem Report
- Hospital/Lab Reports
AutomationEdge’s AI models can verify death certificates and cross-check details with public databases or government records to prevent fraud.
-
General Insurance Claims (Motor/Property)
For motor and general claims, document automation can accelerate survey and approval:
- Claim Form
- Driving License
- FIR Copy
- RC Book
- Surveyor Report
- Odometer Reading
A surveyor’s report can be scanned and processed automatically to calculate damage estimates and initiate settlement.
-
Policyholder Documents (KYC & Bank Details)
Policyholder verification is critical for claim settlement. Automating these documents eliminates repetitive KYC checks:
- KYC Documents (PAN, Aadhaar)
- Policy Certificate
- Cancelled Cheque
- Bank Passbook
AutomationEdge can validate KYC details against government APIs and ensure bank account verification before payment release.
When document automation is implemented:
- Claim TAT drops by 70% (from 7–10 days to less than 48 hours).
- Customer satisfaction scores (CSAT) improve by 25–30% due to faster approvals.
- Fraud detection improves by 20–30% with AI-based document cross-verification.
How AutomationEdge Powers End-to-End Insurance Workflow Automation
AutomationEdge offers Intelligent Document Processing (IDP) and end-to-end claim workflow automation:
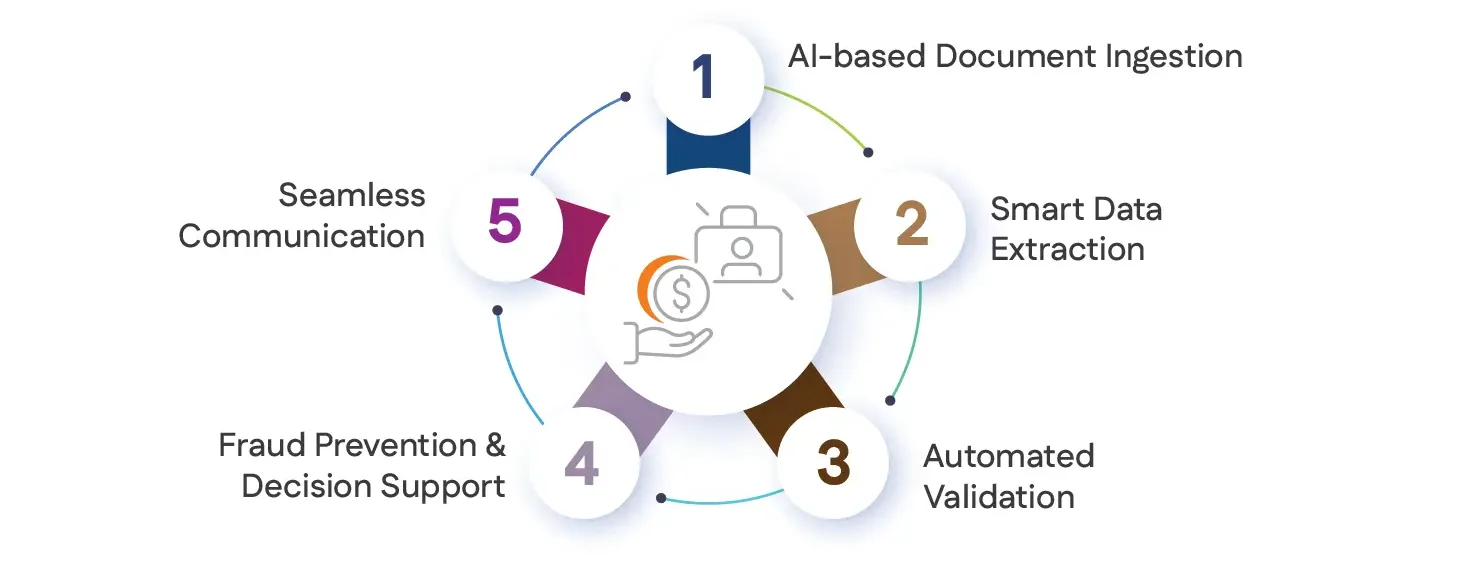
- AI-based Document Ingestion: Classifies claim forms, bills, lab reports, and KYC automatically.
- Smart Data Extraction: OCR + NLP extracts critical information from structured and unstructured documents.
- Automated Validation: Cross-verifies with core insurance systems, government databases, or hospital APIs.
- Fraud Prevention & Decision Support: Rules-based engine approves low-risk claims and flags anomalies.
- Seamless Communication: Keeps customers updated in real-time via email, SMS, or WhatsApp.
Claim Workflow and Opportunities for End-to-End Processing
A traditional claim workflow involves multiple steps:
- Claim submission (document collection & form filling)
- Verification & validation of documents
- Assessment (medical/legal/surveyor evaluation)
- Approval & settlement
Currently, most of these steps are manual or semi-automated, causing:
- Delays due to manual document scrutiny
- High operational costs for back-office processing
- Inconsistent claim experience for policyholders
- Errors and compliance risks due to human oversight
Opportunities for End-to-End Automation
- Document ingestion & data extraction: Automating the capture and classification of claim-related documents.
- Data validation & cross-checking: Matching extracted data with policyholder details in core systems.
- Decision support: Using rule-based automation to approve low-risk claims instantly.
- Empathetic communication: Triggering automated updates via SMS, WhatsApp, or email for policyholders.
Why Insurance Companies Should Prioritize Automating Claim Documents
-
Faster Settlement, Higher Customer Satisfaction
Customers expect instant and empathetic claim resolutions. End-to-end automation reduces settlement time from weeks to hours.
-
Reduced Operational Costs
Automation can cut manual processing costs by 40–60%, freeing up resources for strategic work.

-
Better Fraud Detection & Compliance
AI-based document verification can detect fake claims, ensuring regulatory compliance.
-
Empathetic Claimant Journey
By automating routine tasks, insurers can focus on personalized communication with claimants during critical times.
Best Practices for Implementing Claim Document Automation
To fully realize the benefits of automating claims document processing, insurers should adopt a strategic approach that ensures both efficiency and accuracy throughout the workflow.
-
Standardize Document Formats from the Start
Encourage policyholders, agents, and partners to submit documents in formats that are easily readable by OCR and AI tools. Standardizing formats—such as using typed forms or digital uploads—minimizes errors and speeds up data extraction, making automation more effective from the outset.
-
Seamlessly Integrate with Core Insurance Systems
Connect your automation solutions directly to core platforms like Guidewire or SAP. This integration ensures that data extracted from claim documents flows automatically into your main claims management workflows, eliminating manual data entry and reducing the risk of errors or delays.
-
Prioritize High-Volume Document Types
Begin your automation journey by focusing on the most frequently processed documents, such as discharge summaries, FIR copies, or KYC proofs. Automating these high-impact document types delivers immediate improvements in turnaround time and operational efficiency.
-
Implement AI-Driven Validation
Leverage intelligent document processing (IDP) to automatically cross-check extracted information against trusted sources, such as government APIs or hospital databases. This not only reduces the need for manual verification but also helps detect and prevent fraudulent claims.
-
Monitor Performance and Continuously Optimize
Regularly track key performance indicators like claim turnaround time, data accuracy, and fraud detection rates. Use these insights to identify new opportunities for automation and to refine your processes, ensuring ongoing improvements and maximum return on investment.
By following these best practices, insurers can streamline their claims operations, reduce costs, and deliver a faster, more reliable experience for their customers.
How AutomationEdge Enables Seamless Document Processing
AutomationEdge offers AI + RPA + cognitive document processing to automate claim workflows:
-
Intelligent Document Processing (IDP)
- Extracts data from structured, semi-structured, and unstructured documents (PDFs, images, scanned forms).
- Classifies documents (claim form, death certificate, lab report, etc.) automatically.
- Validates extracted data against policy systems and regulatory databases.
-
End-to-End Workflow Orchestration
- Automates claim intake, verification, and settlement approval.
- Integrates seamlessly with core insurance systems like Guidewire, SAP, or custom legacy apps.
-
Empathetic Customer Communication
- Automatically updates claim status to customers via email, WhatsApp, or chatbots.
-
Fraud Prevention & Compliance
- Uses AI-based anomaly detection to flag suspicious claims.
Conclusion
By automating critical claim documents—health, life, general, and policyholder KYC—insurers can achieve seamless, empathetic, and faster claim processing. AutomationEdge’s cognitive automation makes it possible to process claims end-to-end, delivering both cost efficiency and superior policyholder experience.
Frequently Asked Questions
Forms such as claim intake documents, first notice of loss (FNOL), and reimbursement applications are ideal candidates for automation. These forms are repetitive, data-intensive, and governed by clear rules, making them perfect for intelligent document processing and automation tools.